If you wish to request an urgent clinical appointment or review, you can do this by attending the practice in person or by calling us on 0207-780-8000
Anyone living in Tower Hamlets who is registered with a GP is also entitled access to GP "hubs" across the borough. At these hubs, you will see a Tower Hamlets GP or nurse, face-to-face, with access in the evening and at weekends.
If you contact us to request an appointment and we have reached capacity for the day, our team will often be able to book you a hub appointment where available.
Our local GP hubs are located at:
- Goodman's Field Medical Practice - Field 9, 11 Stable Walk, E1 8ZF
- City Square Medical Group, Cable Street Branch, 445 Cable Street, E1W 3DP
It is extremely important that if you are offered one of these Hub appointments, but cannot kep the appointment then you cancel this as soon as possible by replying with 'Cancel' to the SMS text you will receive from the Hub to confirm your appointment.
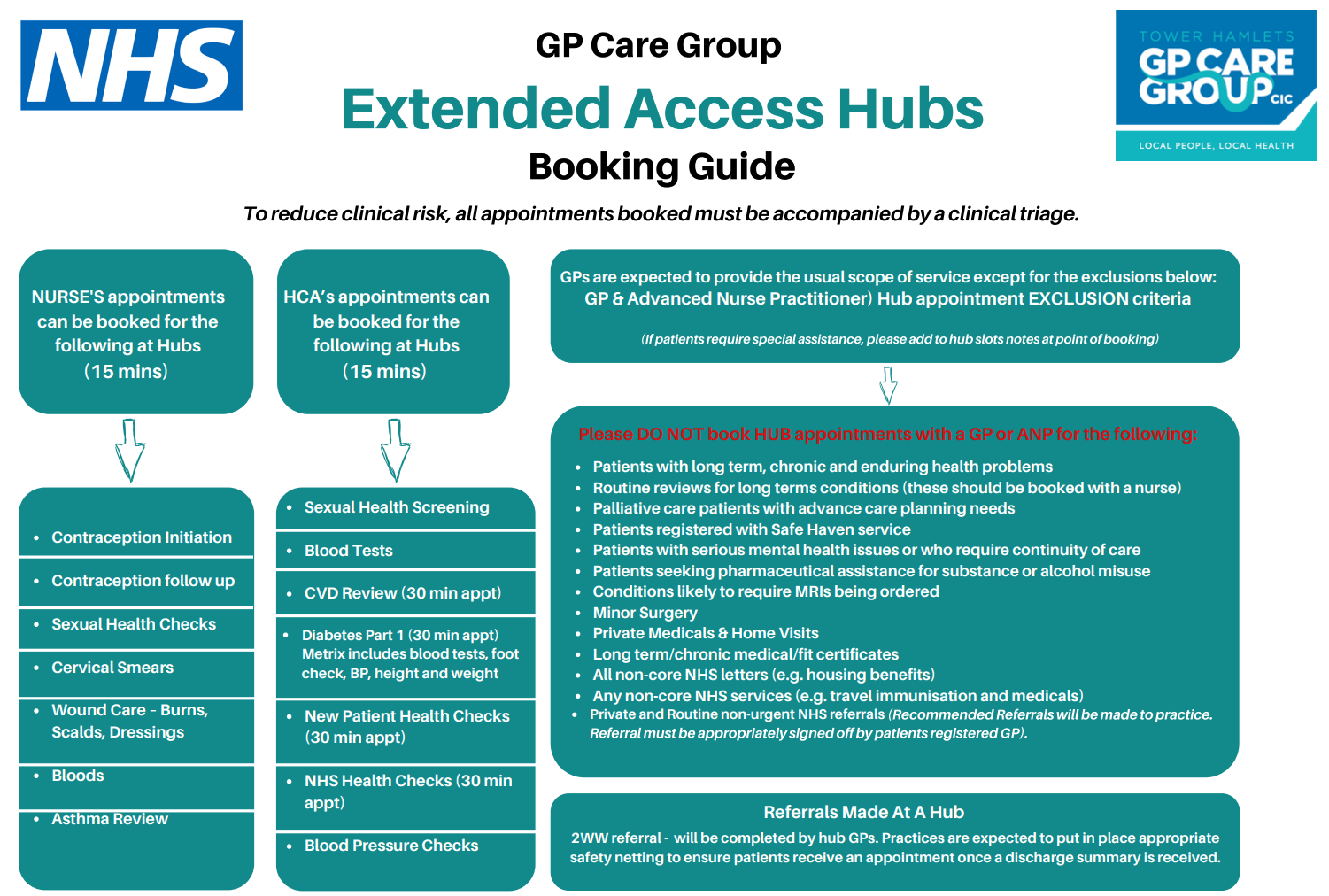
For information on what appointments we can and can't book for, please see below chart:
- Use from any device
- Your data is safe and secure
- Integrates with your NHS App and with our clinical system
- Forms help us gather the information we need from you so that we can offer you the most appropriate help by the right person
In order to keep our clinics running safely and avoid delays for our patients, we kindly ask that all of our patients arrive 5 minutes early to their appointments to give themselves time to check-in at reception.
Nurse appointments
Due to the nature and length of our nurse appointments, if you arrive more than 7 minutes late to appointment you will be asked to re-book on another day.
Jubilee Street Practice is a teaching centre for Barts and the London School of Medicines, and medical students come to the practice as part of their training to become doctors.
Whilst you are at the practice, or when having a telephone consultation, you may be asked whether you would be willing to see or speak to a medical student(s) as well as the healthcare professional you have an appointment with. We would be grateful if you would consider this. By doing so you are contributing to the training of the next generation of doctors.
You may be asked to see a student before your appointment, or to see a student first and then the GP with the student. A doctor will always be in charge and will see you to make sure your problems are dealt with appropriately.
Medical students must keep information you have given them confidential and share it only with other members of the practice team involved in your care. We fully understand that there may be times when you would prefer not to meet medical students. Please let the practice know straight away, it will not affect your treatment in any way.
When contacting us at JSP, there may be times when you are booked a telephone or face to face consultation with our Physician Associates : Tabana Gohar & Aine Begley. To help you understand the role of an physician associate please read below:
What are Physician Associates?
Physician Associates are medically trained health care professionals who work alongside doctors and provide medical care as an integral part of the multidisciplinary team.
What do physician associate do?
They work together with GPs and although they work independently they are supervised and every patient is discussed with a supervising GP. They are experienced and well trained to cover the areas that they work. Most of our baby clinics are run by the Physician Associates.
You might meet them in your GP surgery, on a hospital ward or in the accident and emergency department of your local hospital.
What's so different about physician associates and other specialists?
Physician associates are healthcare professionals who work under the supervision of a senior doctor and can assess, diagnose, and treat patients within certain limits. The difference between Physician associates and other specialist is that they don’t prescribe medication or request X-rays, and they are supposed to supplement and not substitute fully qualified doctors.
How does this affect me?
When booked for an appointment with the Physician Associates, They will always introduce themselves as Physician Associates. However, If you are not happy seeing a physician Associate please inform reception and you can be rebooked to see another clinician, although there may be a wait for an available appointment.
Where Can I find out more?
You can also learn more about Physician Associate in general by visiting
Anyone living in Tower Hamlets who is registered with a GP is also entitled access to CPCS across the borough.
In 2019, Community Pharmacy Consultation Service (CPCS) was created in collaboration with GP surgeries to offer a wider range of services to patients, meaning they do not have to book a GP appointment.
Community pharmacists are highly-skilled practitioners who are experts in medicines and managing minor illnesses. They are qualified to give advice and sometimes prescribe medications for conditions such as:
- Mouth ulcers
- Head lice
- Bites and stings
- Sinusitis
- Sore throats
- Athlete’s foot
- Cold or flu
- Allergies
- Scabies
- Nasal congestion
- Teething
- Blisters
- Oral thrush
- Cold sores
- Warts and verrucae
You will always be told if you have been referred to a community pharmacist with your problem, and you will be guaranteed an appointment within 24 hours of your request. The pharmacist will send a full report back to your GP once you have been seen.
For more information on CPCS please click here to watch a video on 'What can a pharmacist do for you?'
Patient right to a chaperone
Chaperones are there to support patients and staff.
Chaperones should routinely be offered before intimate examinations. Patients can refuse a chaperone, and the patient's acceptance or refusal of this should be noted in the records.
What is a chaperone?
A chaperone is an impartial observer present during an intimate examination of a patient. They will usually be a health professional who is familiar with the procedures involved in the examination. The chaperone will usually be the same sex as the patient.
Intimate examinations
Intimate examinations are examinations of the breast, genitalia and rectum. However, some patients may regard any examination in which the doctor needs to touch or be very close to them as intimate. Example: examination of the fundi using an ophthalmoscope in a darkened room.
Chaperone's role
A chaperone is there for the patient. Their function is to:
- reassure the patient if they experience distress
- protect the patient's dignity and confidentiality at all times
- offer emotional support at an embarrassing or uncomfortable time
- facilitate communication, especially if there is a language barrier
A chaperone also provides a safeguard for both patient and doctor, and can discourage unfounded allegations of improper behaviour. In rare circumstances, the chaperone may also protect the doctor from physical attack.
When to offer a chaperone
A chaperone should be offered routinely before conducting an intimate examination. This applies to both female and male patients.
Some patients may require a chaperone for other examinations too. For example, particularly vulnerable patients or those who have suffered abuse may need a chaperone for examinations where it is necessary to touch or be close to them. In these circumstances, the clinician should use his/her professional judgement about whether to offer a chaperone, depending on the patient's views and level of anxiety.
If the patient refuses a chaperone
Patients have a right to refuse a chaperone. If the clinician is unwilling to conduct an intimate examination without a chaperone, s/he should explain to the patient why s/he would prefer to have one present. S/he may need to offer an alternative appointment, or an alternative doctor, but only if the patient's clinical needs allow this.
No chaperone available/patient unhappy with chaperone
When no chaperone is available or the patient is unhappy with the chaperone offered (for example, if they will only accept someone of the same gender), the clinician can ask the patient to return at a different time, if this is not against their clinical needs. The clinician should try to avoid putting pressure on the patient to proceed without a chaperone or make them feel as if they are inconveniencing him/her.
Children and young people
It is important that children and young people are provided with chaperones. The GMC guidance states that a relative or friend of the patient is not an impartial observer. They would not usually be a suitable chaperone. There may be circumstances when a young person does not wish to have a chaperone. The reasons for this should be clear and recorded.
Chaperone training
All staff at The Jubilee Street Practice are able to undertake a formal chaperone role and are regularly trained so they develop and maintain the competencies required. The training is delivered online so that all formal chaperones understand the competencies required for the role.
Use of chaperones during video consultations
Many intimate examinations will not be suitable for a video consultation. Where online, video or telephone consultations take place, GMC guidance explains how to protect patients when images are needed to support clinical decision making. This includes appropriate use of photographs and video consultations as part of patient care.
Where intimate examinations are performed it is important that a chaperone is offered. Documentation should clearly reflect this. It is important to document who provided the chaperoning. It should also say what part of the consultation they were present for.
Checklist for intimate examinations
Before the examination:
- The clinician explains to the patient why the particular examination is necessary and what it entails so they can give fully informed consent.
- The clinician records the consent discussion in the notes, along with the identity of the chaperone or if a chaperone was offered but declined.
- If possible, a chaperone of the same gender as the patient is used.
- The chaperone is allowed to hear the explanation of the examination and the patient's consent.
During the examination:
- Patients' privacy is ensured during the examination and when they are dressing and undressing, for example by using screens and gowns/sheets.
- The chaperone is positioned where they can see the patient and how the examination is being conducted.
- The clinician explains what s/he is going to do before s/he does it and seeks consent again if the examination will differ from what s/he has told the patient before.
- The clinician stops the examination if the patient asks him/her to.
- Personal remarks are avoided.
- It can be helpful to invite the patient to tell the clinician if the examination becomes uncomfortable. While performing the examination, the clinician watches for any signs of pain or discomfort and checks that the patient agrees for the clinician to continue.
After the examination:
- The chaperone should leave the room following the examination and once the patient is dressed so the consultation can continue in private.
The NHS, including Jubilee Street Practice, are facing huge demands. To help us to help as many of you as possible, we are asking that anyone with internet access contacts us online. It is essential that our phone lines are kept as free as possible for emergencies and the elderly and vulnerable, who really cannot use online services. In November, we moved to our new booking system and to using e-consult as our preferred contact method. Currently we are still receiving:
- Approx. 2,000 calls a week (425 a day)
- And only approx. 500 e-Consults a week (100 a day)
Some benefits of using e-consult:
- Increased efficiency and time saving on administration so we can help more patients each day
- Improved information gathering so we can get you booked with the right person at the right time
- Saves you waiting in a phone queue of up to an hour!
So next time you need our help, PLEASE CONTACT US ONLINE
From 1st November 2021 we are making improvements to the way you can access your GP practice, safely and securely.
The information you provide in your e-Consult will be reviewed by a clinician, who will assess the clinical urgency.
Consultations will be prioritised according to need:
- Urgent appointments will be reserved for the most unwell patients who we feel need a same day assessment
- Less urgent problems will be grouped into those needing an assessment within 48 hours and those that can wait up to a week
- Routine follow ups and long-term condition reviews we will aim to offer an appointment within 14 days
Depending on the type of problem, the appointment offered may be by telephone, video or face to face. Alternatively, we may signpost you to a different service if they are better placed to help, or provide you with advice by text if a consultation is not necessary.
For telephone and video appointments, we will send a text offering an appointment within the next 14 days. If you need a face-to-face appointment, a member of the reception team will call you to arrange a suitable time. (We will also call you back on a landline if you do not have a mobile number or IT access).
If you are offered a telephone appointment, we will advise you of the date and a one hour time-slot when we will call, making it easier to plan your day. If we cannot reach you at your allocated appointment time, we will try a second time. If we still cannot contact you, we will send a text message asking you to contact us again on a different day if the appointment is still needed.
As well as GPs and practice nurses, at Jubilee Street we have a large team of clinicians with whom you may be offered a consultation. This includes a clinical pharmacist, a physician associate, a musculoskeletal practitioner, a mental health practitioner, a midwife, and a cardiovascular nurse. We may also, when appropriate, refer you to one of our local pharmacies for a consultation with a pharmacist under the national CPCS (community pharmacy consultation service). Community pharmacists are trained to offer treatment and advice for a range of illnesses and ailments.